
КАТЕГОРИИ:
Архитектура-(3434)Астрономия-(809)Биология-(7483)Биотехнологии-(1457)Военное дело-(14632)Высокие технологии-(1363)География-(913)Геология-(1438)Государство-(451)Демография-(1065)Дом-(47672)Журналистика и СМИ-(912)Изобретательство-(14524)Иностранные языки-(4268)Информатика-(17799)Искусство-(1338)История-(13644)Компьютеры-(11121)Косметика-(55)Кулинария-(373)Культура-(8427)Лингвистика-(374)Литература-(1642)Маркетинг-(23702)Математика-(16968)Машиностроение-(1700)Медицина-(12668)Менеджмент-(24684)Механика-(15423)Науковедение-(506)Образование-(11852)Охрана труда-(3308)Педагогика-(5571)Полиграфия-(1312)Политика-(7869)Право-(5454)Приборостроение-(1369)Программирование-(2801)Производство-(97182)Промышленность-(8706)Психология-(18388)Религия-(3217)Связь-(10668)Сельское хозяйство-(299)Социология-(6455)Спорт-(42831)Строительство-(4793)Торговля-(5050)Транспорт-(2929)Туризм-(1568)Физика-(3942)Философия-(17015)Финансы-(26596)Химия-(22929)Экология-(12095)Экономика-(9961)Электроника-(8441)Электротехника-(4623)Энергетика-(12629)Юриспруденция-(1492)Ядерная техника-(1748)
Treatment
|
|
|
|
Nonsurgical
In all cases, the patient should be initially resuscitated, given broadpectrum intravenous antibiotics and fully heparinized. As yet, the twin goals of mesenteric revascularization and resection of nonviable bowel can only be achieved by surgical means.
Surgery is indicated in all patients with peritonitis. Angiography in patients without peritonitis may demonstrate NOMI or MVT. In NOMI, treatment is nonoperative and depends on optimizing cardiac output and treating underlying conditions such as sepsis. Intramesenteric arterial infusion of papaverine at a dose of 30 to 60 mglr may be beneficial.
Up to 65% of patients who have undergone cardiac surgery have had symptomatic improvement within hours when diagnosed early.
If MVT is diagnosed at angiography, intra-arterial thrombolytic therapy has been given successfully. Nonoperative management by full anticoagulation for acute MVT is feasible when the initial diagnosis is certain and when the bowel infarction has not led to transmural necrosis and bowel perforation. The morbidity, mortality, and survival rates are similar in cases of surgical and nonoperative management.
Other reported endovascular procedures for acute intestinal ischemia include fenestration and stent placement in aortic dissection, angioplasty and stenting in an acute occlusion in a patient with chronic mesenteric insufficiency, and angioplasty alone. This contrasts with an increasing use of angioplasty for chronic mesenteric ischemia.
SURGICAL
Laparotomy is indicated in patients with peritonitis after rapid resuscitation. The first step is to assess the degree and extent of bowel viability. Free, foul smelling peritoneal fluid is a sign of advanced necrosis even if perforation has not occurred. Ischemic bowel has a characteristic appearance with loss of its normal sheen. It is dull, gray in color and flabby in tone without any peristalsis. Infarcted bowel is purplish black in color, often friable and perforated. In many cases the bowel ischemia will be so extensive and advanced that no further surgical treatment is undertaken and palliative care given. Where there is hope of sufficient bowel viability, revascularization should be performed before any bowel resection is considered. After successful revascularization, previously precarious segments of intestine may recover and resection of clearly ischemic bowel can then take place.
SMA embolectomy. The proximal portion of the SMA is dissected free from the surrounding fat and lymphatic tissue just as it emerges from the pancreatic neck into the base of the mesentery. Approximately 3 to 4 centimeters of artery is cleared, with care taken not to damage the branches. Heparin (5000 units) is given intravenously. A transverse arteriotomy is made and a 3F or 4F embolectomy catheter is passed proximally and distally to clear the embolus and reestablish vigorous pulsatile flow. If proximal flow cannot be established, SMA thrombosis is likely and reconstructive surgery will be required.
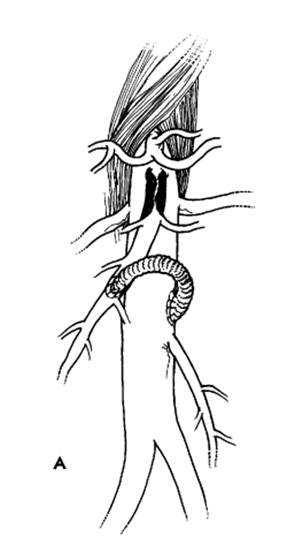
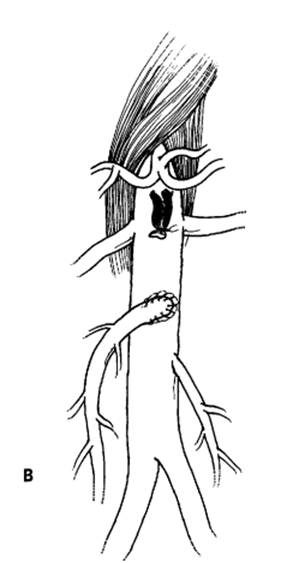
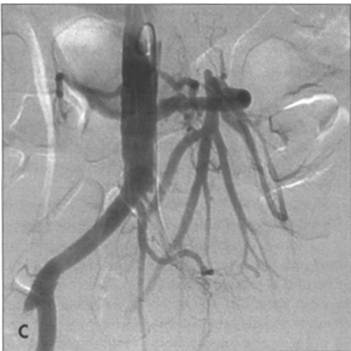
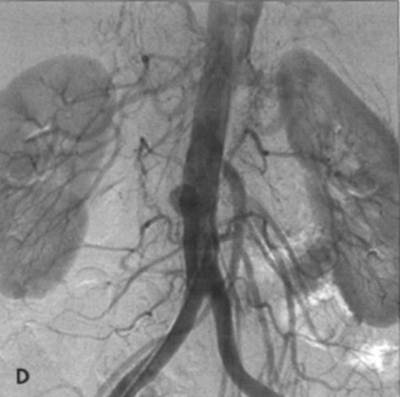
FIG. A - Schematic representation of revascularization of the SMA with: bypass taking care to avoid kinking and obs-
truction B - Or re-implantation of SMA into the aorta. C - Angiographic appearance of aorto-SMA bypass with vein graft.
There is co-existing left common iliac occlusion. D - Angiographic appearance of re-implanted SMA into aorta, which has
a smal l saccular aneurysm at the site of occluded vein graft (aortoceliac bypass).
|
|
|
|
|
Дата добавления: 2014-12-23; Просмотров: 472; Нарушение авторских прав?; Мы поможем в написании вашей работы!